In September 2021, an article entitled “Challenges of Sarcoidosis and Its Management” (Drent et al., 2021) was published in the prestigious New England Journal of Medicine. This article, written by two active members on FSR’s Scientific Advisory Board, Marjolein Drent MD, PhD, and Elliott Crouser MD, FSR Scientific Advisory Board Chair, provides a detailed overview of what sarcoidosis is, challenges in diagnosis, and complexity and diversity of disease progression and manifestations that impact treatment pathways. This is a great article to share with your team of physicians to help them have a better understanding of the disease, especially for those physicians that do not typically treat patients with sarcoidosis. There are also several diagrams (called “algorithms”) which could be a helpful tool to bring to your sarcoidosis treating doctor to help you weigh the best course for treatment.
As you probably already know, sarcoidosis is an inflammatory disease that can affect almost any organ. Researchers don’t yet know what causes sarcoidosis. Up until a few years ago, there was very little insight into what causes sarcoidosis or why and how granulomas form. Unlike other diseases, there are no useful animal models of sarcoidosis. The current theory is that people with a genetic predisposition for sarcoidosis encounter some type of trigger. This trigger could be an infection or an exposure to something in the environment. So far, moldy places and some work environments have been identified as triggers. Some cases of sarcoidosis go away on their own (“spontaneously remit”), while other people develop into chronic cases that involve multiple organs and dramatically change their quality of life.
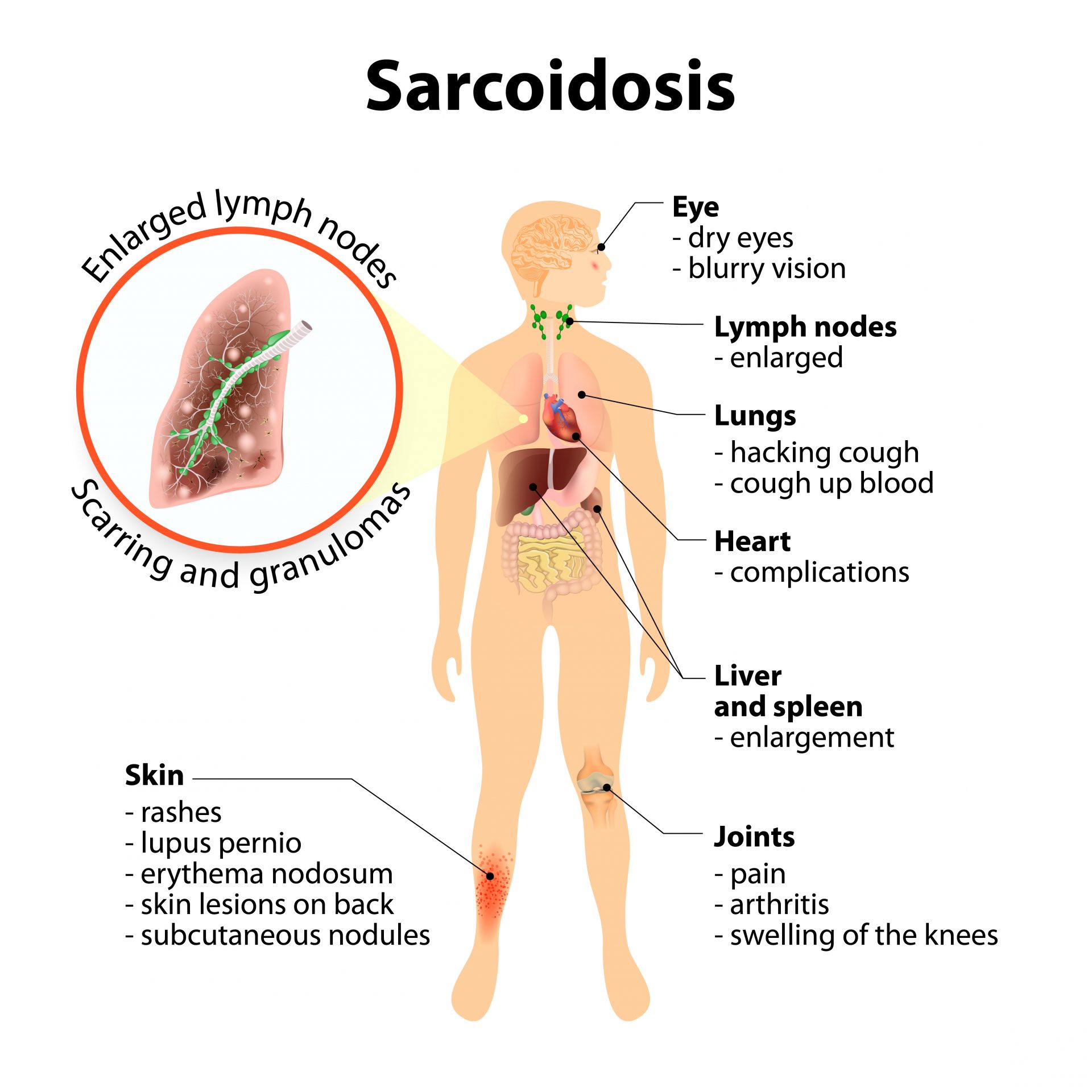
It’s difficult to have an accurate sense of just how many people have sarcoidosis. This is because sarcoidosis is hard to diagnose. In fact, there’s not even consensus among doctors how to diagnose sarcoidosis. The authors of this article describe sarcoidosis as “chameleon-like.” It can show up in any organ, although most often the lungs are involved. This article provides a “diagnostic pathway” tool for clinicians to help improve diagnosis. The reason that diagnosis is complicated is that patients have a range of symptoms—from shortness of breath to fatigue to cognitive impairment. There are three criteria for diagnosing sarcoidosis: having symptoms of the disease, finding granulomas in a biopsy, and ruling out other diseases. Diagnostic tools include checking angiotensin-converting enzyme (ACE) levels in blood serum, CT scans, FDG-PET scans, MRI, and biopsies. However, physicians need to be aware that a negative test does not mean that sarcoidosis is not involved.
In addition to sarcoidosis being difficult to diagnose, it’s equally challenging to treat. Diagnosis of sarcoidosis is more complicated to diagnose than an illness like strep throat: where a single test usually provides a certain diagnosis, and an antibiotic is known to cure it. Deciding when and how to treat a patient “is complex and cannot be standardized,” according to the authors. This complexity of the disease makes sarcoidosis difficult to predict in terms of natural disease progression (some patients experience resolution without treatment while others have a relentless progression). Additionally, it is difficult to determine the effect of the disease on patient quality of life and related costs (a patient’s inability to work and the effect on a family when a patient is unable to function normally etc.) This is hard for both sarcoidosis patients and their doctors. In this article, the authors attempt to measure the effects of sarcoidosis in terms of organ function, but most patients tend to be more interested in addressing chronic fatigue, chronic pain, etc. Additionally with sarcoidosis, there has yet to be conclusive data on how effective different treatments are.
As a baseline, doctors should consider the risk of organ failure (or death) and how badly a patient’s quality of life is affected by the disease when deciding to start treatment and in determining the best treatment pathway. The goal of treatment is to suppress inflammation in sarcoidosis-impaired organs and to optimize quality of life by addressing sarcoidosis related symptoms such as chronic pain, severe fatigue and impaired cognitive functions. Unfortunately, “successful” treatments don’t always make patients feel better. The general consensus is to start with glucocorticoids (also known as steroids). These drugs have many side effects. For those patients who need longer courses of treatment, or who cannot tolerate glucocorticoids, there are many other options. All these medications have risks and possible side effects. You should encourage your physician to read this article as it lays out different treatment pathways and questions they should consider in pursuing a course of treatment.
Another area of emphasis in this review was the importance of optimizing healthy life-style choices. For instance, a growing body of evidence indicates that regular exercise is additive to medical treatments in terms of improving disease symptoms and even improves organ function. Other factors, such as avoidance of emotional stress and adherence to a healthy diet should be emphasized by healthcare providers. Medications are not always the best solution!
This article provides a synopsis of our current understanding of the disease, paths for diagnosing, and considerations in selecting treatments. There is a great need for future study, including identifying better biomarkers to help predict disease progression. The authors suggest that better identifying the genetic components of the disease will be helpful. They also point to a need for new ways to identify the disease and a great need for more and better treatment options. There are research tools now available including a new disease model for labs and new genetic techniques. These new tools are providing a window into the mechanisms of sarcoidosis and are allowing for new therapeutic targets, new biomarkers, and research to test novel therapies. Once again, this is a great reference to share with your treating physicians so they have a better understanding the disease and can identify the best treatment pathway for you.
This blog is sponsored by Mallinckrodt Pharmaceuticals, Boehringer Ingelheim, and aTyr as part of our sarcoidosis awareness campaign.
Summary Article Authors:


References Drent, M., Crouser, E. D., & Grunewald, J. (2021). Challenges of Sarcoidosis and Its Management. New England Journal of Medicine, 385(11), 1018–1032. https://doi.org/10.1056/nejmra2101555
