Sarcoidosis of the Skin
Cutaneous Sarcoidosis is the second most common form of sarcoidosis and occurs in approximately 30% of patients.¹ Cutaneous Sarcoidosis may appear differently in different individuals as raised bumps, patches of red or darkened skin, or open sores. Cutaneous sarcoidosis is often called ‘the great mimicker’ because it can look like many other conditions that impact the skin. The face is a common site, as are tattoos and scars.
Symptoms2
Diagnosis3
Sarcoidosis is a diagnosis of exclusion, meaning that other infections and causes must be ruled out before sarcoidosis can be diagnosed.
- Tuberculous Test. Doctors will often conduct a tuberculin skin test (PPD) which injects a small amount of the tuberculin protein into the skin. Then, 48-72 hours later, your doctor will measure your skin’s reactivity. It is possible for you to have a false positive to the PPD, but also a false negative. If this is suspected, your clinician may use a secondary test to confirm results. Sometimes a blood test is used instead of the skin test.
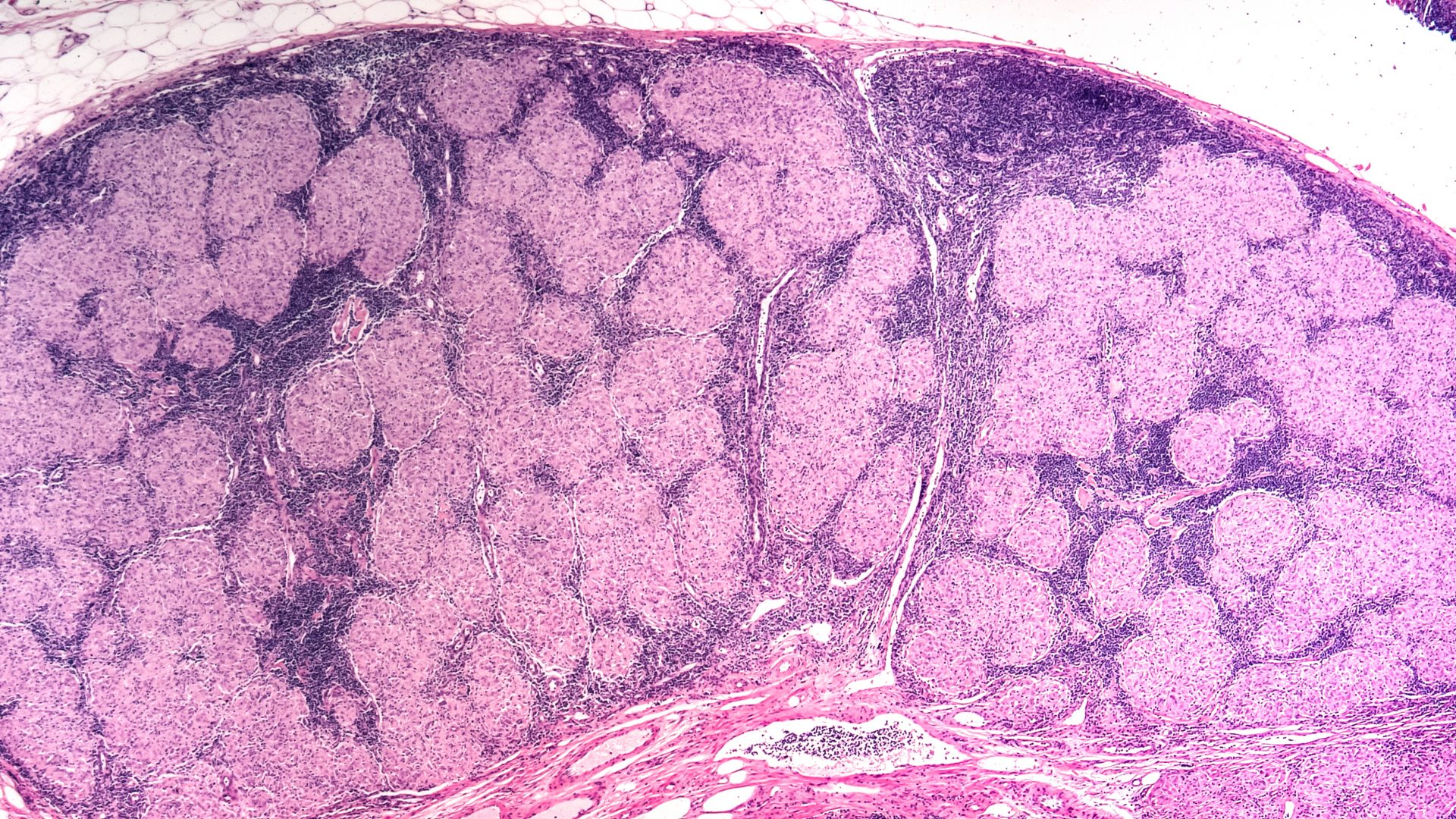
- Biopsy. If your clinician suspects sarcoidosis, he or she will take a small biopsy of the skin. This biopsy allows them to confirm or rule out granulomatous formations associated with sarcoidosis. Occasionally, more than one biopsy is required.

Systemic treatments
Systemic treatments are treatments that are designed to not only target the skin but may also address any additional manifestations of the disease. These treatments may include:
Emerging therapies on the horizon
- JAK inhibitors. JAK inhibitors are janus kinase inhibitors that bind or reduce the activity of enzymes (JAK1, JAK2, JAK3, TYK2) in the body. There have been several studies looking at JAK inhibitors as a new potential therapy for cutaneous sarcoidosis, both topically and systemically. JAK inhibitors have a number of side effects and come with a black box warning. 5,6,7
Other Things to Consider8
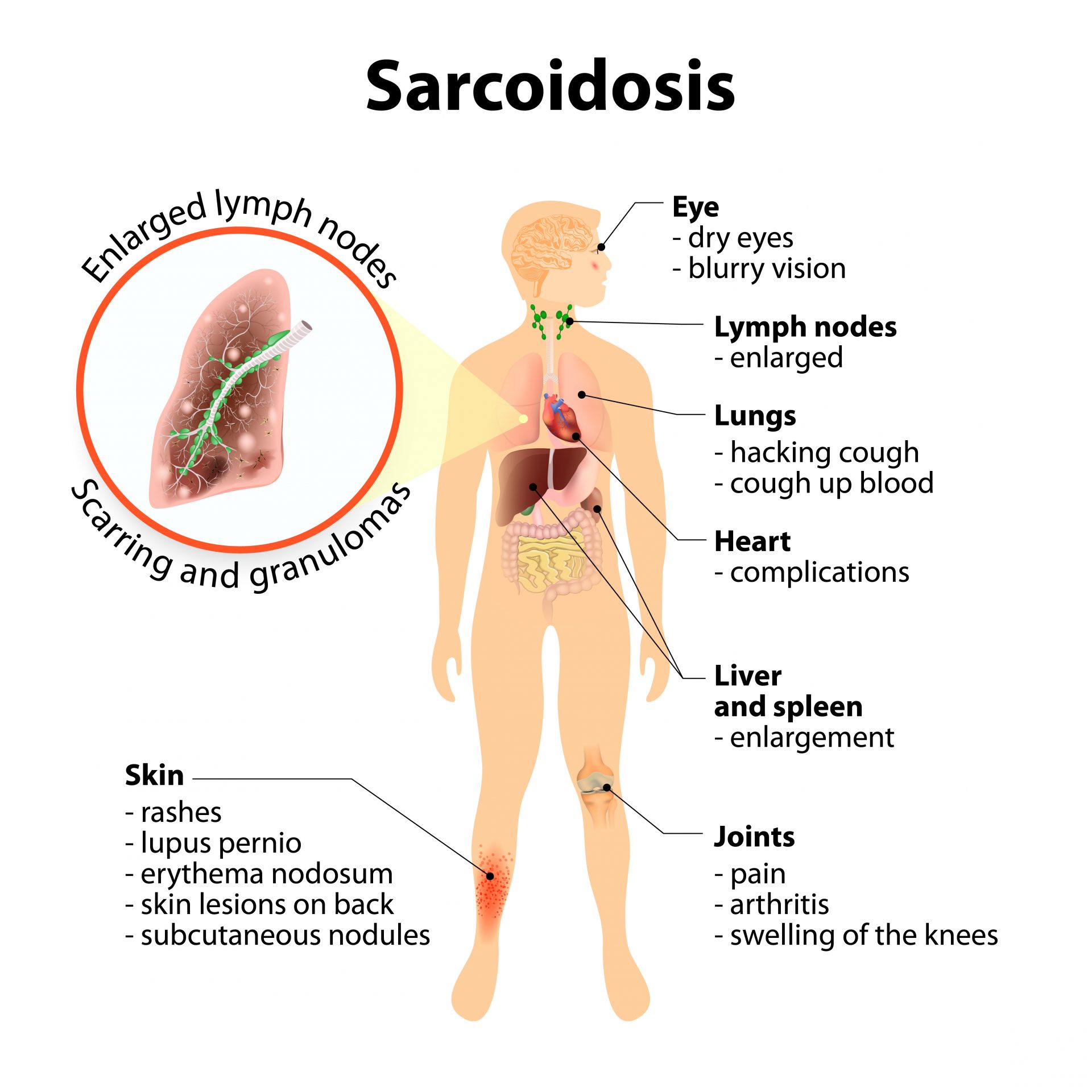
- Patients with sarcoidosis, including skin sarcoidosis, usually have some degree of disease beyond the skin.
-90% of those living with sarcoidosis have lung involvement or pulmonary sarcoidosis.
- Diagnosis of skin sarcoidosis should be followed by a number of other tests to rule out other manifestations of sarcoidosis including:
-Chest X ray
-Ophthalmological (eye) exams
-Cardiac Screenings
-Blood work
Questions to ask your doctor
- What should I expect from a skin biopsy?
- If I am diagnosed with sarcoidosis of the skin, should I be concerned with having sarcoidosis somewhere else in my body?
- How do I know if the therapy you prescribed is not working?
- How often should I plan for a recheck visit?
- What should I look for that may indicate a flare or advancement of my disease?
Watch Overview: Skin Sarcoidosis
Sources
1. Samtsov AV. Cutaneous sarcoidosis. Int J Dermatol. 1992;31:385-91
2. Haimovic A, Sanchez M, et al. “Sarcoidosis: A comprehensive review and update for the dermatologist. Part I. Cutaneous disease.” J Am Acad Dermatol. 2012; 66:699.e1-18.
3. Misha Rosenbach (2017). Sarcoidosis (cutaneous sarcoidosis) Dermatology Advisor https://www.dermatologyadvisor.com/home/decision-support-in-medicine/dermatology/sarcoidosis-cutaneous-sarcoidosis/
5. Tofacitinib Treatment and Molecular Analysis of Cutaneous Sarcoidosis. Damsky W, Thakral D, Emeagwali N, Galan A, King B.N Engl J Med. 2018 Dec 27;379(26):2540-2546. doi: 10.1056/NEJMoa1805958.
6. Treatment of cutaneous sarcoidosis with tofacitinib: A case report and review of evidence for Janus kinase inhibition in sarcoidosis. Talty R, Damsky W, King B.JAAD Case Rep. 2021 Aug 20;16:62-64. doi: 10.1016/j.jdcr.2021.08.012. eCollection 2021
7. Janus kinase inhibitors offer promise for a new era of targeted treatment for granulomatous disorders.
Rosenbach M.J Am Acad Dermatol. 2020 Mar;82(3):e91-e92. doi: 10.1016/j.jaad.2019.06.1297. Epub 2019 Jul 3.
